Let’s Dig Deeper! Functional Medicine and why it’s so important for personalised care
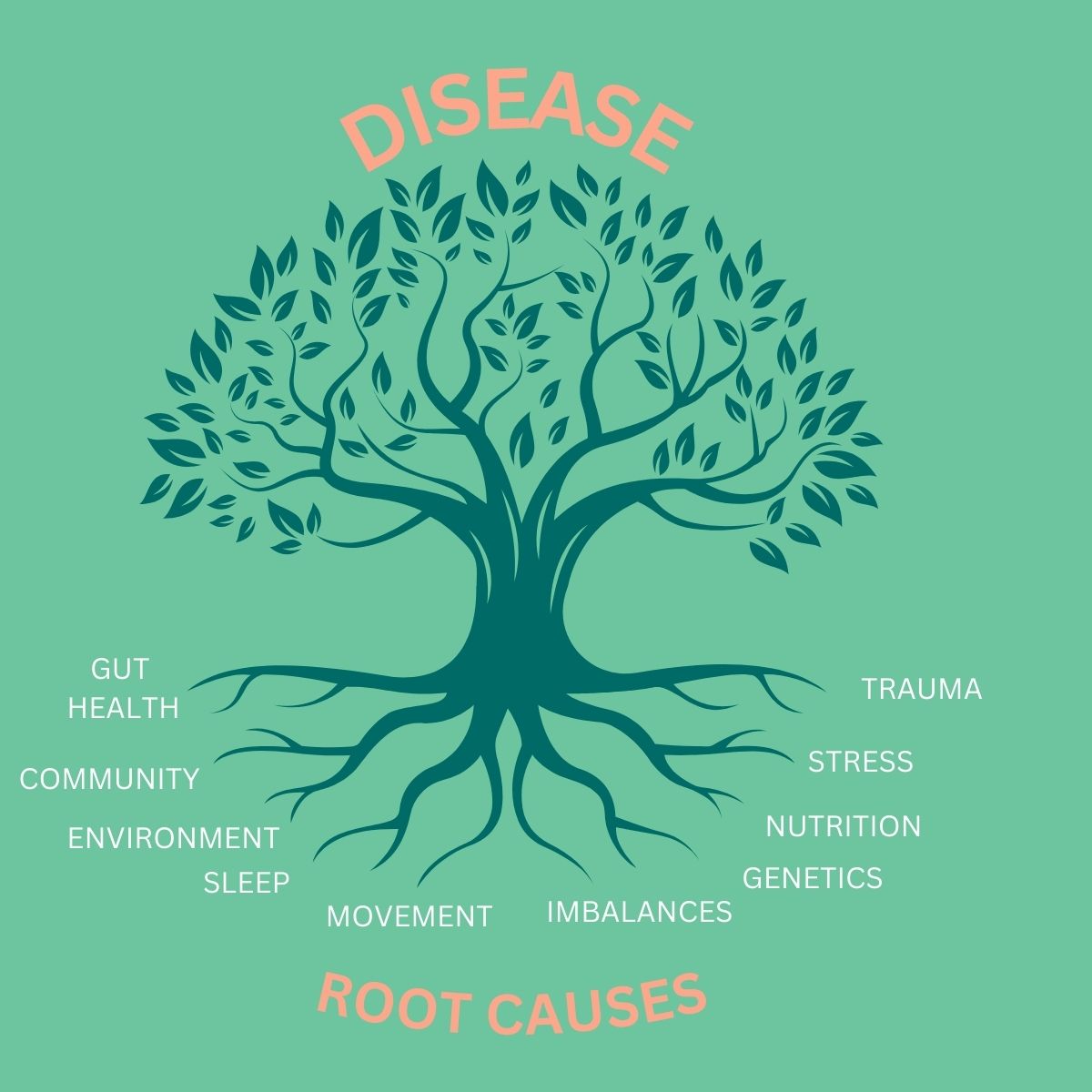
So how does functional medicine differ? What functional medicine does is find out what the underlying root is of a condition, as well as individualising personal care plans to allow for optimal management of chronic illnesses or to improve wellness in general. Chronic diseases are those that persist over a long period of time — they may not be curable, but they are treatable in fact we know that 80% of chronic diseases are treatable.
Even with the huge amounts of spending on healthcare, we’re still seeing rises in chronic diseases. In the US, 60% of adults will have one chronic disease, and about 44% will have at least two chronic diseases, often both requiring medication. And the UK is not too far behind this. Clearly, there is a gap in the way healthcare is managed at the moment, and in the needs of the patients. Functional medicine aims to close that gap and find personalised approaches to reduce someone’s risk of chronic illnesses and improve their health overall.
Within functional medicine we really try to uncover some hidden messages within the health history, to identify clues that we can draw upon in the treatment plan. Traditionally, in conventional medicine, there’s been a hierarchical structure where doctors are seen as all-knowing. Functional medicine aims to flatten that hierarchy and work in conjunction with the patient, focusing on their goals and treating them according to their needs and perspectives.
Functional medicine also has access to expanded testing options. Whilst we’re fortunate to have free access to healthcare in this country, with a wide range of testing available. However, the limited spending the NHS has means that testing is often based on the most cost-effective strategies for the population. Functional medicine can fill that gap by understanding if there’s anything further we can do, why treatment isn’t working, or why a patient still isn’t feeling quite right. However, expanded treatment options aren’t always necessary because often a full evaluation and understanding of a patient’s lifestyle is enough. When we work in partnership with the patient, functional medicine can often address their needs without the need for extra testing.
The core of functional medicine is truly lifestyle medicine. It involves looking at a person’s stress management, relaxation, exercise, nutrition, and relationships. It really delves into those factors and helps patients to use these to manage their health and wellness. Sleep, movement, nutrition and relationships may not be addressed initially within conventional medicine, but they can often reveal gaps that need attention. It’s essential to consider all aspects of someone’s life when designing a treatment plan and to recognise that even low-cost, modifiable factors can have a big impact.
The key part of a functional medicine approach is the mental, emotional, and spiritual health of the patient. It’s important to understand someone’s sense of purpose, their relationships, and how they handle emotional situations. This is crucial when developing a treatment plan. Without considering these aspects, the plan might not feel relevant to the patient, and they may not engage with it fully. It’s important to note that mental, emotional, and spiritual aspects of health should not be dismissed as “low-impact.” In fact, these aspects can be just as important as physical interventions. Many conventional medical approaches, such as medication, are often the first line of defence, but in functional, integrative and lifestyle medicine, we recognise the power of mind-body techniques like meditation, gratitude practices, and yoga. These practices are empowering because they give individuals a sense of control over their health and well-being.
On the left side of the matrix, we look at predisposing factors, including inherited issues, past trauma, injuries, procedures, and toxic exposures. Stressful life events and emotional states also play a role. By looking at these factors in this manner, we can better understand the path forward in managing their conditions.
Finally, when integrating functional medicine into your healthcare, it’s essential to view the entire picture. This includes working with your GP and collaborating on care. For example, hypertension management is critical for preventing strokes. Medications like blood pressure medication may be necessary to reduce risks, but the goal is to work on lifestyle factors to eventually reduce or eliminate the need for medication.
Dr Elizabeth Thompson